Autism spectrum disorder (ASD) is a multifaceted neurodevelopmental condition characterized by challenges in social interaction, communication, and behavior. From the early signs of delayed speech to the complexities of sensory sensitivities, ASD presents a spectrum of symptoms that vary widely among individuals. While the exact causes of ASD remain elusive, researchers have been exploring various factors that may contribute to its development and manifestation. One such area of interest is the gut microbiome – the diverse community of microorganisms that inhabit our digestive tract. Far from just aiding in digestion, the gut microbiome plays a pivotal role in maintaining overall health, influencing everything from immune function to mental well-being. This intriguing connection between gut health and neurological conditions like ASD has sparked a wave of research aimed at understanding how the gut microbiome might impact the development and management of ASD symptoms. As we delve deeper into this fascinating realm, let’s explore the significance of the gut microbiome and its potential implications for individuals with ASD.

The Connection Between Gut Biome and Autism:
Recent studies have brought to light a compelling link between the gut microbiome and autism spectrum disorder (ASD), suggesting that the microbial communities residing in our digestive tract may play a role in the development and expression of ASD symptoms. One such study, published in the journal Cell, conducted comprehensive analyses of gut microbiota composition in children with ASD and neurotypical children. The findings revealed significant differences in the abundance and diversity of gut bacteria between the two groups, indicating that alterations in the gut microbiome could be associated with ASD. Similarly, research published in Frontiers in Cellular Neuroscience provided further evidence of this connection, reporting lower microbial diversity in the gut of children with ASD compared to their neurotypical counterparts. These findings have sparked interest and speculation about the potential mechanisms underlying the relationship between gut health and ASD. By shedding light on the intricate interplay between the gut microbiome and neurological conditions like ASD, these studies have paved the way for further exploration into the role of gut bacteria in shaping brain development and function.

Established Studies on the Effect of Gut Biome in Autistic Children:
Research examining the impact of the gut microbiome on autism spectrum disorder (ASD) symptoms and behavior has yielded valuable insights into the potential role of gut health in influencing neurological conditions. Several key studies have provided compelling evidence of the link between the gut microbiome and ASD, shedding light on both the methodologies used and the outcomes observed. For instance, a landmark study published in the Journal of Autism and Developmental Disorders conducted fecal microbiota transplantation (FMT) in children with ASD, aiming to modulate their gut microbiota and assess changes in behavior. The results revealed improvements in gastrointestinal symptoms and behavioral issues following FMT, suggesting a potential therapeutic avenue for managing ASD symptoms.
Similarly, a systematic review and meta-analysis published in Nutritional Neuroscience evaluated the effects of probiotic supplementation on ASD-related symptoms. The analysis found that probiotics, which are beneficial bacteria known for promoting gut health, were associated with improvements in gastrointestinal symptoms and certain behavioral aspects of ASD. These findings underscore the potential of targeting the gut microbiome as a means of ameliorating ASD symptoms and improving overall well-being in affected individuals.
Differences in Gut Biome of Autistic Individuals:
When comparing the gut microbiota composition of individuals with ASD to neurotypical individuals, researchers have identified specific differences that may contribute to the manifestation of ASD symptoms. These disparities in gut microbiome profiles encompass various factors, including diet, genetics, and environmental influences. For example, a study published in the Proceedings of the National Academy of Sciences examined the gut microbiota of individuals with ASD and found alterations in microbial taxa associated with carbohydrate metabolism and amino acid biosynthesis. These findings suggest potential metabolic differences in the gut microbiome of individuals with ASD, which could impact nutrient absorption and metabolic processes.
Moreover, research has highlighted the role of environmental factors, such as antibiotic use and dietary patterns, in shaping the gut microbiome of individuals with ASD. A study published in Autism Research investigated the impact of early-life antibiotic exposure on gut microbiota composition and ASD risk. The results indicated that antibiotic use during infancy was associated with alterations in gut microbiota diversity and an increased likelihood of ASD diagnosis later in childhood. These findings underscore the complex interplay between environmental factors, gut microbiome composition, and the development of ASD, highlighting the importance of considering multiple influences when studying this intricate relationship.
Understanding the Disparities:
The altered gut microbiome observed in individuals with autism spectrum disorder (ASD) has prompted researchers to explore the underlying mechanisms that contribute to these disparities. While the exact reasons remain elusive, several hypotheses have emerged to elucidate the relationship between the gut microbiome and ASD.
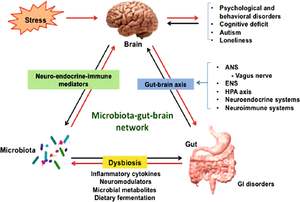
1. Gut-Brain Axis Communication: One compelling theory suggests that disruptions in the communication between the gut and the brain, known as the gut-brain axis, may play a role in ASD. This bidirectional communication pathway involves intricate signaling between the gut microbiota, the nervous system, and the immune system. Dysregulation of the gut-brain axis could lead to aberrant signaling that influences neurological function and behavior, potentially contributing to the development and expression of ASD symptoms.
2. Immune System Dysregulation: Another hypothesis implicates immune system dysregulation in shaping the gut microbiome of individuals with ASD. Emerging evidence suggests that immune dysfunction, characterized by chronic inflammation and altered immune responses, may be associated with ASD. Disruptions in immune function could impact the composition and activity of gut microbiota, leading to dysbiosis and potentially exacerbating ASD-related symptoms.
3. Environmental Influences: Environmental factors, such as diet, antibiotic exposure, and environmental toxins, may also contribute to alterations in the gut microbiome of individuals with ASD. Dietary patterns high in processed foods and low in fiber can disrupt the balance of gut bacteria, while antibiotic use can alter microbial diversity and composition. Additionally, exposure to environmental toxins, such as heavy metals and pollutants, may disrupt gut microbiota and contribute to gut dysbiosis in individuals with ASD.
4. Genetic Predisposition: Genetic factors may also play a role in shaping the gut microbiome of individuals with ASD. Studies have identified genetic variations associated with ASD that could influence gut microbiota composition and function. These genetic predispositions, combined with environmental influences, may contribute to the unique gut microbiome profiles observed in individuals with ASD.
5. Early Life Influences: The early developmental period, including prenatal and early postnatal life, is critical for the establishment and maturation of the gut microbiome. Disruptions during this sensitive period, such as maternal factors, mode of delivery, and infant feeding practices, may have lasting effects on gut microbiota composition and diversity. Early-life influences on the gut microbiome could potentially contribute to the development of ASD later in life.
In summary, understanding the disparities in the gut microbiome of individuals with ASD requires consideration of multiple factors, including the complex interplay between the gut-brain axis, immune system dysregulation, environmental influences, genetic predispositions, and early-life experiences. Further research is needed to unravel the intricate mechanisms underlying these disparities and their implications for ASD pathophysiology and management.
Strategies for Modulating the Gut Biome:
Improving gut health in individuals with autism spectrum disorder (ASD) involves implementing interventions aimed at restoring microbial balance and promoting a healthy gut environment. Several approaches, including dietary changes, probiotics, prebiotics, and fecal microbiota transplantation, show promise in modulating the gut microbiome and potentially alleviating ASD-related symptoms.
Dietary Changes: Diet plays a crucial role in shaping the gut microbiome, making dietary modifications an essential component of gut health interventions. For individuals with ASD, adopting a diet rich in fiber, nutrients, and beneficial bacteria can help support a diverse and resilient gut microbiota. In the context of an Indian diet, incorporating the following dietary recommendations can promote gut health:
Probiotic-Rich Foods: Include probiotic-rich foods such as yogurt (curd), buttermilk (lassi), and fermented vegetables like pickles in daily meals. These foods contain live beneficial bacteria that can help replenish and maintain a healthy gut microbiome.
High-Fiber Foods: Increase fiber intake by consuming whole grains like brown rice, whole wheat bread, and lentils (dal). Fiber serves as a prebiotic, nourishing beneficial bacteria in the gut and promoting microbial diversity and fermentation.
Fruits and Vegetables: Incorporate a variety of fruits and vegetables, such as spinach, carrots, bananas, and berries, into the diet. These foods provide essential nutrients, antioxidants, and fiber that support gut health and overall well-being.
Limit Processed Foods and Sugars: Minimize consumption of processed foods and sugars, opting instead for homemade meals prepared with fresh, locally sourced ingredients. Processed foods and sugars can disrupt gut microbiota balance and contribute to inflammation and metabolic dysfunction.
Traditional Spices: Emphasize traditional spices like turmeric, cumin, and ginger, known for their anti-inflammatory properties and potential benefits for gut health. These spices not only add flavor to dishes but also provide medicinal properties that support digestive health and immune function.
By incorporating these dietary changes into daily routines, individuals with ASD can promote a healthy gut microbiome and potentially mitigate gastrointestinal symptoms and behavioral issues associated with the disorder. However, it’s essential to consult with healthcare professionals or nutritionists to tailor dietary recommendations to individual needs and preferences.
In summary, strategies for modulating the gut biome in individuals with autism spectrum disorder encompass dietary modifications aimed at promoting microbial balance and gut health. By incorporating probiotic-rich foods, increasing fiber intake, consuming a variety of fruits and vegetables, limiting processed foods and sugars, and emphasizing traditional spices, individuals with ASD can support a diverse and resilient gut microbiome. These dietary interventions, tailored to an Indian context, offer actionable steps for promoting gut health and overall well-being in individuals with ASD.
Conclusion:
The gut microbiome emerges as a pivotal player in the intricate landscape of autism spectrum disorder (ASD), offering new avenues for understanding and potentially managing this complex condition. Through a series of studies, researchers have illuminated the significance of the gut microbiome in ASD, revealing alterations in microbial composition and diversity that may contribute to the development and expression of ASD symptoms.
The gut-brain connection serves as a compelling framework for understanding the interplay between gut health and neurological function, highlighting the potential for bidirectional communication between the gut microbiome and the brain. While the mechanisms underlying this connection remain elusive, hypotheses involving the gut-brain axis, immune system dysregulation, environmental influences, genetic predispositions, and early-life experiences offer valuable insights into the multifaceted nature of ASD.
As we navigate this evolving field, it is evident that further research is needed to elucidate the mechanisms underlying the gut-brain connection in ASD and to develop targeted interventions for improving the gut health of individuals with ASD. By unraveling the complexities of the gut microbiome and its implications for ASD, researchers can pave the way for innovative therapies and personalized interventions that address the diverse needs of individuals on the autism spectrum.
In closing, the journey towards understanding the gut microbiome in ASD is just beginning, offering hope and promise for enhancing the lives of individuals with this condition. Through continued collaboration, innovation, and dedication, we can unlock new insights into the gut-brain connection and harness the potential of gut-focused interventions to support the well-being of individuals with ASD.
References:
Kang, D. W., Adams, J. B., Gregory, A. C., Borody, T., Chittick, L., Fasano, A., … & Krajmalnik-Brown, R. (2017). Microbiota Transfer Therapy alters gut ecosystem and improves gastrointestinal and autism symptoms: an open-label study. Microbiome, 5(1), 10.
Coretti, L., Paparo, L., Riccio, M. P., Amato, F., Cuomo, M., Natale, A., … & Berni Canani, R. (2018). Gut microbiota features in young children with autism spectrum disorders. Frontiers in Microbiology, 9, 3146.
Liu, S., Li, E., Sun, Z., Fu, D., Duan, G., Jiang, M., … & Cui, Y. (2019). Altered gut microbiota and short chain fatty acids in Chinese children with autism spectrum disorder. Scientific Reports, 9(1), 287.
Sharon, G., Cruz, N. J., Kang, D. W., Gandal, M. J., Wang, B., Kim, Y. M., … & Krajmalnik-Brown, R. (2019). Human gut microbiota from autism spectrum disorder promote behavioral symptoms in mice. Cell, 177(6), 1600-1618.
Dash, S., Clarke, G., Berk, M., & Jacka, F. N. (2015). The gut microbiome and diet in psychiatry: focus on depression. Current Opinion in Psychiatry, 28(1), 1-6.
Tomova, A., Husarova, V., Lakatosova, S., Bakos, J., & Vlkova, B. (2015). Gastrointestinal microbiota in children with autism in Slovakia. Physiological Research, 64(Supplementum 3), S321-S331.
Mulle, J. G., Sharp, W. G., & Cubells, J. F. (2013). The gut microbiome: a new frontier in autism research. Current Psychiatry Reports, 15(2), 337.
Support for the MEDA Foundation is crucial in advancing research and interventions aimed at understanding and addressing the complexities of autism spectrum disorder (ASD) and its potential connection to the gut microbiome. By supporting the MEDA Foundation, individuals, organizations, and communities can contribute to groundbreaking research initiatives that seek to unravel the mechanisms underlying ASD and explore innovative strategies for improving the lives of individuals affected by the condition. With a focus on collaboration, innovation, and advocacy, the MEDA Foundation plays a vital role in fostering partnerships between researchers, healthcare professionals, policymakers, and individuals and families affected by ASD. Through their dedication to funding research, raising awareness, and promoting evidence-based interventions, the MEDA Foundation serves as a beacon of hope for individuals with ASD and their loved ones. By rallying support for the MEDA Foundation, we can collectively work towards a future where individuals with ASD receive the support, understanding, and opportunities they deserve.










